Mental health challenges among U.S. military personnel have grown into an undeniable crisis.
Rising rates of anxiety, depression, PTSD, and adjustment disorders now impact a significant portion of the armed forces.
Contributing factors include prolonged post-9/11 combat deployments, the prolonged stressors of the COVID-19 pandemic, and persistent cultural stigma around mental illness in uniformed service.
Data collected over the last few years show a troubling surge in diagnoses, exposing gaps in support systems meant to care for those who serve.
Annual Diagnoses and Trends
Between 2019 and 2023, mental health diagnoses among active-duty service members reached crisis levels.
More than 541,000 individuals were diagnosed with at least one mental health disorder.
Nearly 255,000 were diagnosed with multiple conditions, resulting in a staggering total of 966,227 reported diagnoses over the five-year period.
A closer year-by-year analysis paints an even more urgent picture. Mental health diagnoses surged by 40% across the active-duty population.
This sharp rise cannot be dismissed as a fluke or temporary spike. Instead, it highlights persistent and compounding stressors linked to warzone deployments, prolonged exposure to trauma, isolation during pandemic lockdowns, and administrative pressures within the military.
Specific diagnostic categories reveal deeper layers of concern. The most dramatic change occurred in anxiety-related disorders, which climbed 77% during the study period. Depression and PTSD diagnoses also grew at alarming rates.
- Total mental health diagnoses (2019–2023): 966,227
- Personnel with at least one diagnosis: 541,000+
- Diagnosed with multiple conditions: Nearly 255,000
- Overall increase in diagnoses: 40%
- Increase in anxiety disorders: 77%
- Depression and PTSD: Consistent upward trajectory
Mounting evidence points to several contributing factors:
- Prolonged post-9/11 deployments without sufficient decompression
- Cultural stigma deterring early mental health intervention
- Increased operational tempo amid global instability
- Psychological aftermath of COVID-19 lockdowns and social isolation
- Inadequate resources for reintegration support
While more service members are now stepping forward for mental health care, medical units and military health systems are stretched thin.
Facilities often lack the capacity to manage the volume and complexity of these cases.
In many instances, personnel must wait extended periods before accessing care, and those with severe or comorbid conditions often require structured intervention such as an intensive outpatient program or mental health treatment plan.
Most Common Diagnoses

Mental health data collected between 2019 and 2023 reveals that certain conditions consistently affect service members in large numbers. Adjustment disorder emerges as the most prevalent diagnosis, with nearly 283,000 reported cases during the five-year span.
This condition typically affects individuals responding to significant life changes or stressors and is especially common among personnel in their first three years of service. In many cases, the stress of transitioning into military life, adapting to rigid command structures, and dealing with relocation or separation from family becomes overwhelming.
- Adjustment disorder: ~283,000 cases
- Depression (2023 alone): ~40,000 new cases
- PTSD: Nearly doubled by 2023
- Anxiety: Increased consistently post-COVID
Anxiety and depression remain persistent challenges. The post-pandemic environment saw a spike in anxiety disorders as troops dealt with isolation, unpredictable schedules, restricted movement, and delayed leave cycles.
Military culture often prizes stoicism, which may delay early intervention and lead to more severe symptoms over time.
Depression cases added to the psychological burden in large numbers, with nearly 40,000 new cases documented in 2023 alone.
In some instances, these diagnoses overlapped with PTSD, creating complications in symptom tracking and treatment planning.
PTSD nearly doubled by 2023. Repeated exposure to combat, life-threatening scenarios, and moral injury often leads to long-term symptoms.
- Major depressive disorder
- Traumatic brain injury (TBI)
- Substance use disorders
These combinations often require structured care plans. In more severe instances, service members benefit most from participation in an intensive outpatient program mental health framework, which allows for daily clinical support while enabling partial duty continuation.
Demographic and Branch Differences

Patterns of mental health diagnoses differ across branches, genders, and age groups. Service environment, mission tempo, and occupational stress levels all play a role in these variations.
Some trends highlight potential gaps in support or exposure to higher psychological demands.
- Army: Highest overall rate of diagnoses
- Navy: Highest rates for depressive, bipolar, and personality disorders
- Coast Guard: Most acute stress disorder cases, often tied to fast-paced rescue and enforcement missions
Gender-based differences show that female personnel are disproportionately affected by PTSD, with rates nearly double those seen in males.
Age and service experience matter too. Younger service members, particularly those in the early stages of their careers, face elevated risks.
Lack of experience with stress regulation, combined with difficult duty assignments, contributes to higher adjustment, anxiety, and depression rates.
- PTSD rates in females: Nearly 2x higher than in males
- Young, early-career members: Most affected by adjustment and anxiety disorders
- Junior enlisted ranks: Show highest levels of untreated or emerging symptoms
These disparities underline the importance of tailoring mental health outreach and care strategies to meet the needs of specific groups.
A one-size-fits-all approach does not account for the nuanced stressors each branch or demographic faces.
Long-Term and Historical Context

Patterns seen in recent years echo findings from historical analyses. A 2008 RAND Corporation study of post-deployment mental health revealed sobering insights.
Approximately 18.5% of personnel met criteria for depression or PTSD, while 19% experienced symptoms consistent with traumatic brain injury.
Even then, major systemic barriers prevented timely and effective care.
- Concerns about confidentiality
- Fear of damaging career prospects
- Side effects of medications
- Lack of trust in available care systems
Despite improvements in screening and awareness, similar concerns persist. Cultural stigma within the military still discourages many from seeking help. Peer pressure, command expectations, and the fear of being labeled “unfit” can lead to long delays between symptom onset and diagnosis.
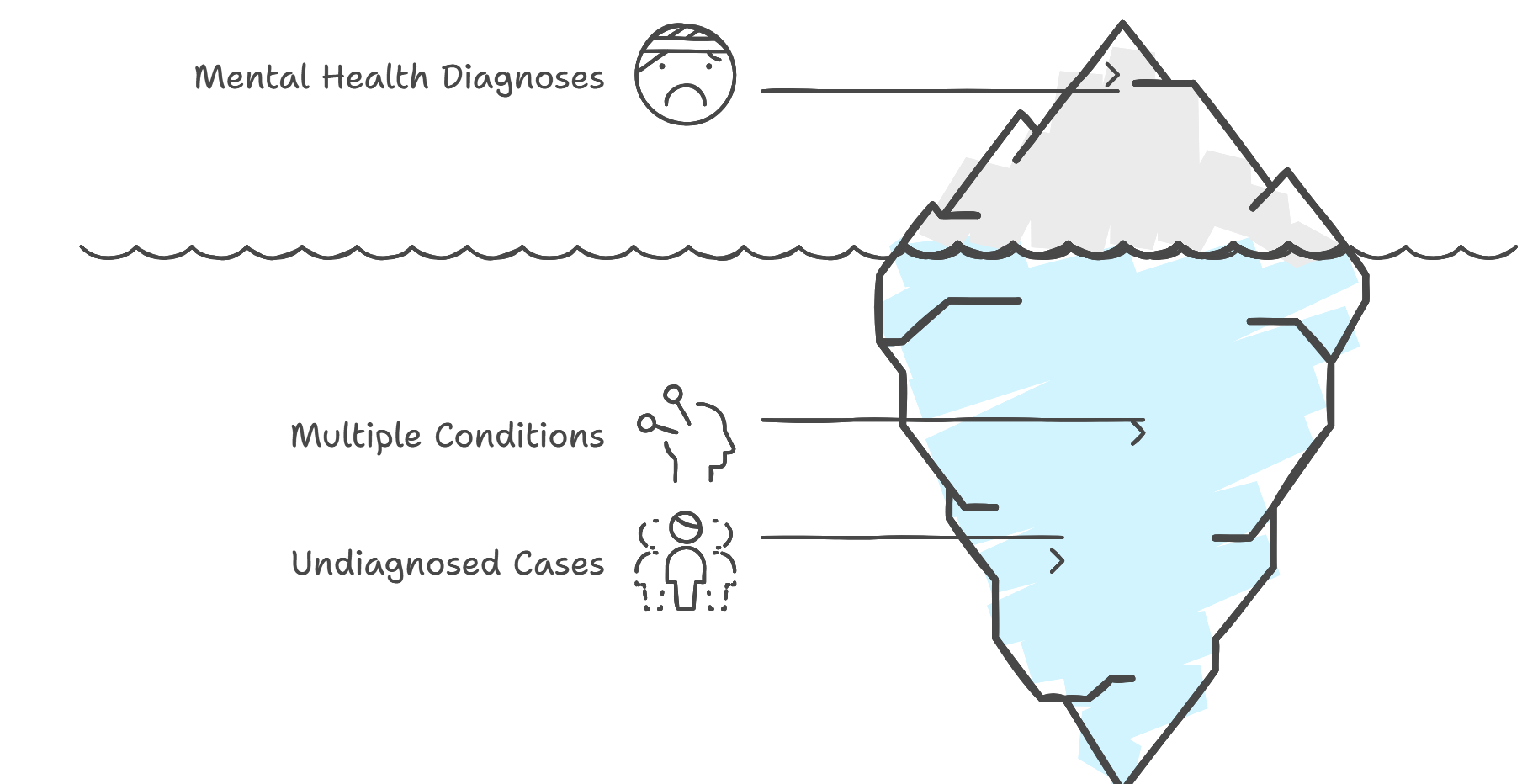
While PTSD rates have declined slightly from their highest wartime levels, they remain troublingly high. Many experts believe the actual rates are underreported due to fear of retribution or dismissal.
- Stigma delaying early care
- Cultural resistance to acknowledging psychological injuries
- Limited access to long-term care after deployment
Current trends must be viewed not only as present-day issues but also as extensions of unresolved problems dating back to past conflicts. The institutional memory of trauma, and the failure to fully address it, continues to affect today’s force.
Impacts on Military Readiness and Health Systems

The surge in mental health diagnoses directly affects operational effectiveness and medical readiness.
Hospitalization data from 2023 shows that mental health disorders consumed 54.8% of all inpatient bed days within military hospitals.
- Mental health usage: 54.8% of all hospital bed days
- Physical injury usage: Less than half by comparison
Such high bed usage impacts not only those receiving care but also others waiting for critical services. Military hospitals are often understaffed or lack mental health specialists, leading to longer wait times and fragmented care.
Another challenge lies in staffing. The ongoing shortage of trained mental health professionals continues to cripple military treatment facilities.
Many regions lack adequate numbers of counselors, psychologists, and psychiatrists trained in trauma-informed care or familiar with military culture.
- Shortage of clinicians specializing in combat trauma
- Delayed referrals and overbooked treatment teams
- Gaps in continuity of care during deployments or transfers
Financial costs further complicate the issue. Historical data places the cost of PTSD and depression treatment between $4 and $6.2 billion for just two years.
Initial treatment for TBI in 2007 was estimated between $591 million and $910 million, figures likely higher in today’s economy.
The Bottom Line
Mental health disorders among U.S. troops are increasing at an alarming pace, cutting across rank, gender, branch, and age.
Data paints a stark picture, one of escalating need, overstretched resources, and consequences for operational effectiveness.
Early recognition, cultural change, and expanded treatment availability are essential if the military is to preserve both its strength and the well-being of those who serve. Visibility is only the beginning, real solutions require sustained commitment.
Related Posts:
- Everything You Need to Know About Military Mental…
- VA Disability 5-Year Rule Explained - How It Affects…
- Common Health Challenges Veterans Face and How to…
- How Many WW2 Veterans Are Still Alive? Will There Be…
- How Many Navy Fleets Does the US Have in 2025?
- How Many Generals Does the U.S. Military Have in 2025?







